IDE Research Columns
Column
Surgical Productivity Change During and After the COVID-19 Pandemic in Japan

Yuichi WATANABE
Institute of Developing Economies, JETRO
February 2025
What are the effects of the coronavirus disease 2019 (COVID-19) pandemic on routine healthcare services other than COVID-19 treatments? We investigated the surgical productivity change during and after the pandemic in Japan by examining the case of a large university hospital. Our studies revealed that the COVID-19 pandemic negatively affected the improvement of surgical productivity in the short term. However, the change in surgical productivity did not suffer from the state of emergency during the pandemic. Furthermore, no evidence indicated that the pandemic had any lasting effects on reducing surgical productivity during the post-pandemic period. Our implications for surgical practice and healthcare policy would be valuable lessons for future pandemics.
Background and Motivation
The novel coronavirus disease 2019 (COVID-19) pandemic was first identified in Wuhan, China in early 2020, over four years ago. To control the COVID-19 pandemic, the Japanese government declared its first state of emergency in several prefectures in April 2020, which was then expanded nationwide. The government subsequently declared three more states of emergency against the COVID-19 pandemic in 2021. The state of emergency encouraged citizens to refrain from nonessential moves and to stay home. In response to the COVID-19 pandemic, healthcare resources were intensively allocated to COVID-19 treatments, which consequently decreased the available resources for other healthcare areas and quality of their services. For example, the number of elective surgical procedures were significantly reduced, and the blood products for surgery became short in supply because of voluntary self-quarantine. Further, more healthcare professionals were engaged in measures to combat COVID-19, causing shortages of manpower for routine health services. These COVID-19 treatments, combined with extreme routine healthcare service restrictions, may have resulted in the collapse of the entire healthcare system. The effects of the COVID-19 pandemic and the states of emergency in Japan on routine healthcare services other than COVID-19 treatments remain quantitatively unclear. A series of our studies attempted to investigate the changes in surgical productivity during and after the COVID-19 pandemic in Japan by examining the case of a large university hospital (Nakata et al. 2022a; Nakata et al. 2022b; Nakata et al. 2024).
Hypothesis
Surgical productivity is the performance of surgeons in operating rooms, where they use labor and capital inputs to produce a certain output (Coelli et al. 2005). Efficient surgeons are assumed to maximize the output while minimizing the utilization of the inputs. A productive entity is usually termed a decision-making unit (DMU) in our model, representing the dynamic productivity change of a DMU between two time periods.1 We considered surgical treatments as routine health services that were not directly associated with COVID-19 treatments. We hypothesized that the COVID-19 pandemic and the states of emergency significantly reduced the surgical total factor productivity, and the decreased surgical productivity exerted a significant lasting effect during the post-pandemic periods.
Data and Variables
Our studies utilized clinical and claims data extracted from surgical records in the electronic medical record system of Teikyo University Hospital in the Tokyo metropolitan area. The Teikyo University Hospital contains 1,152 beds and reports an annual surgical volume of approximately 9,000 cases in 13 surgical specialties. This hospital, one of the largest special functioning hospitals in Japan, is located in a prefecture where a state of emergency was initially declared by the Japanese government and was acutely affected by the COVID-19 pandemic. A currently practicing physician extracted information on all the surgical procedures performed in the main operating rooms from April 1 to September 30 for each year from 2016 to 2022. We collected data only for six months each year due to research budget and time constraints. Our data include the date of surgery, surgical specialty, patient’s age and sex, start and end time of surgery (yielding total surgical time), name of the responsible surgeon, number of assisting physicians, and classification of “K codes” corresponding with surgical fees.
We defined a DMU as the highest academically ranked surgeon who controlled all the inputs and outputs (i.e., senior surgeon) in Nakata et al. (2022a), and as a surgical specialty department in Nakata et al. (2022b) and Nakata et al. (2024). We also defined output as the total surgical fees for each surgery, whereas labor and capital inputs were defined as the number of medical doctors who assisted with the surgery and the duration of the surgical operation from skin incision to closure, respectively (Figure 1). The surgical fees for all surgeries are categorized into over 1,000 K codes in the fee schedule, such as K000–K939, and each surgical procedure is assigned to one or a combination of K codes. The Japanese government determines the fee schedule. Surgeons select from various surgical procedures, which have a range of fees. They strive to achieve the maximum surgical fee through an optimal combination of selected surgical procedures best suited to the patient’s condition, as well as effective capital and labor utilization.
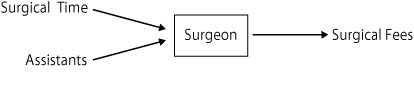
Figure 1. Association Between the Inputs and Output Through a DMU
Source: Created by the Authors
Results and Findings
We initially revealed significantly decreased surgical productivity from 2019 to 2020 based on the quarterly comparison. Our results indicate that the COVID-19 pandemic significantly reduced the improvement of surgical productivity by decreasing the efficiency of surgeons (Nakata et al. 2022a). Our comparative analysis of the effects of the states of emergency from 2019 to 2020/2021 for the study period of consecutive 10 (or 11) days in a month revealed that the surgical productivity significantly progressed both during the states of emergency and non-states of emergency. However, no statistically significant differences in productivity change were observed between states of emergency and non-states of emergency, indicating that the states of emergency against the COVID-19 pandemic in Japan did not affect surgical productivity (Nakata et al. 2022b). Furthermore, focusing on the long-term effects of the COVID-19 pandemic on surgical productivity changes, we determined that the productivity change of all surgical procedures was not significantly different between the pre-pandemic (2016 – 2019) and post-pandemic (2020 – 2022) periods, despite the decreased total surgical volume per year by approximately 10% in the post-pandemic period compared to the pre-pandemic period (Nakata et al. 2024). These results indicate that surgical productivity fully recovered to the pre-pandemic level by 2022 despite a short-term productivity regression in 2020 (Nakata et al. 2022a).
Clinical and Policy Implications
In response to the Japanese government’s first state of emergency declaration, Teikyo University Hospital reduced the number of elective surgeries by 20% to 50% during the first half of April 2020. The restriction was eased to approximately 70% in early May and was removed by the end of May 2020. Some surgeons continued to work in the emergency rooms because of an emergency physician shortage, but these hospital policy changes reflected the resource allocation toward COVID-19 treatments. Hence, the pandemic mostly caused negative productivity changes. However, the hospital did not restrict the number of elective surgeries in the subsequent states of emergency in 2021. The clinical restriction lasted only for approximately 50 days during our study period, thereby exerting minimal effects on surgical productivity. Further, another study revealed that the decline in the number of physician visits due to the spread of COVID-19 reduced by almost half after the second state of emergency declaration, and that the staying-at-home effect did not persist (Kumagai 2021). This may confirm our findings of surgical productivity recovery after the pandemic in Japan. Our results are valuable lessons learned from our experience during the COVID-19 pandemic. Based on their implications for surgical practice and healthcare policy, we can better deal with a similar pandemic in the future.
Author’s Note:
This column is based on Nakata et al. 2022a, Nakata et al. 2022b, and Nakata et al. 2024.
Note:
- We employed the Malmquist index (MI) model as an advanced form of data envelopment analysis to assess surgical productivity changes during and after the COVID-19 pandemic. Please refer to Färe et al. (1994) and Coelli et al. (2005) for details.
References
Coelli, Timothy J., D.S. Prasada Rao, Christopher J. O’Donnell, and George E. Battese. 2005. An Introduction to Efficiency and Productivity Analysis. Second Edition. New York: Springer.
Färe, Rolf, Shawna Grosskopf, Björn Lindgren, and Pontus Roos. 1994. “Productivity Developments in Swedish Hospitals: A Malmquist Output Index Approach.” In Data Envelopment Analysis: Theory, Methodology, and Applications, edited by Abraham Charnes, William W. Cooper, Arie Y. Lewin, and Lawrence M. Seiford, 253–272. Dordrecht: Springer.
Kumagai, Narimasa. 2021. “The Impact of the COVID-19 Pandemic on Physician Visits in Japan.” Frontiers in Public Health 9: 743371. https://doi.org/10.3389/fpubh.2021.743371
Nakata, Yoshinori, Yuichi Watanabe, and Akihiko Ozaki. 2022a. “Productivity Change of Surgeons During the Coronavirus Disease 2019 Pandemic in Japan.” INQUIRY: The Journal of Health Care Organization, Provision, and Financing 59: 1–6. https://doi.org/10.1177/00469580221128737
Nakata, Yoshinori, Yuichi Watanabe, and Akihiko Ozaki. 2022b. “Surgical Productivity Did Not Suffer Despite the States of Emergency Against the COVID‑19 Pandemic in Japan: A Rretrospective Observational Study.” BMC Health Services Research 22: 1267. https://doi.org/10.1186/s12913-022-08669-w
Nakata, Yoshinori, Yuichi Watanabe, and Akihiko Ozaki. 2024. “Surgical Productivity Recovery After the COVID-19 Pandemic in Japan.” Frontiers in Public Health 12: 1302732. https://doi.org/10.3389/fpubh.2024.1302732
* Thumbnail image: 143177296 Surgical Team (gchutka / Getty Images)
** The views expressed in the columns are those of the author(s) and do not represent the views of IDE or the institutions to which the authors are attached.

