IDE Research Columns
Column
International Nurse Migration from India: Time to Say Goodbye?
Yuko TSUJITA
Institute of Developing Economies, JETRO
January 2023
International nurse migration has increased recently in response to the growing global demand for nurses. India is among the major nurse-sending countries, and it fills the shortages in destination countries. However, the country itself is experiencing the shortage of nurses. Emigration from India is mainly explained by the gap between the private and public sectors in terms of remuneration, working conditions, and workplace environment in the country. The coronavirus disease 2019 (COVID-19) pandemic has further increased the demand for nurses. Unless the working conditions of nurses are improved and decent work is created in India, the country will continually remain a major nurse-supplying country and will present with shortages.
Growing Global Demand for Nurses
The global nursing shortage is well recognized before the COVID-19 pandemic outbreak. According to the World Health Organization (WHO), approximately 9 million nurses will be further required by 2030 (WHO 2020a). Among other factors, population aging in several developed countries has contributed to the higher demand for nurse workforce. However, domestic self-sufficiency is challenging to achieve due to several reasons, such as the turnover of the existing nursing workforce and the small number of younger workforces caused by declining birth rate. To address the shortage of nurses, some developed countries chose to recruit nurses from international sources. On average across Organisation for Economic Co-operation and Development (OECD) countries, 15.8% of all nurses were born abroad in 2015/16 (OECD 2020).
India as a Nurse-Sending but Shortage Country
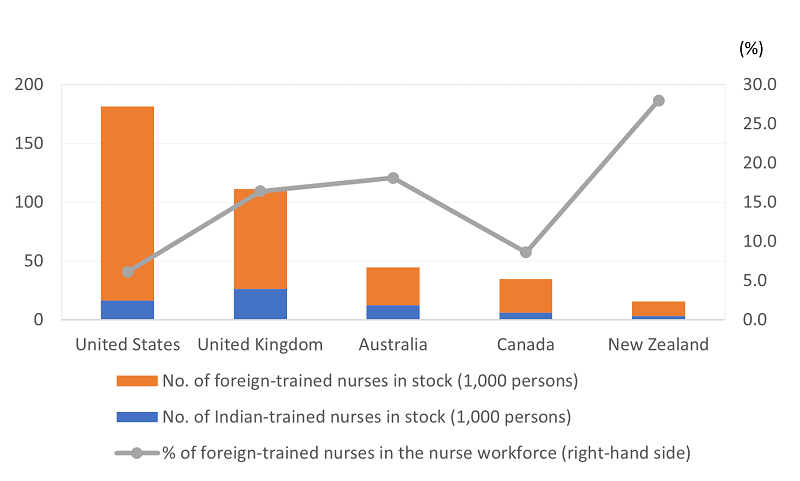
India is among the main nurse-sending countries. It has the second highest number of nurses after the Philippines in 2015/16 (OECD 2020), and approximately 88,000 of their nurses are sent to OECD countries. The main destinations are English-speaking countries, such as the United Kingdom, United States, and Australia (Figure 1). Approximately 640,000 nurses are working abroad, including in Gulf countries, which are the main destinations of nurses (Irudaya Rajan and Nair 2013).
However, India also experiences shortage of nurses. The number of nurses per 10,000 population was only 17.3 in 2018. Meanwhile, those in world and high-income countries were 36.9 and 107.7, respectively (WHO 2020b). In particular, the shortage of nurses in rural areas in India is alarming. That is, 73 of 640 districts in the country have no registered nurses at all (Anand and Fan 2016).
Who Are More Likely to Go Abroad?
Based on our nursing school alumni survey in the state of Tamil Nadu, the type of nursing school is the most influential factor of international migration. Nurses who graduated from private nursing schools are more likely to work abroad than their counterpart nurses who studied nursing in government nursing schools. Private nursing school graduates are more likely to work in private hospitals. This notion is particularly true in Tamil Nadu where state government hospitals traditionally recruited nurses who graduated from government institutions until in recent years. Private hospitals generally offer lower salary, and they have inferior working conditions and less secured job in terms of employment contract than government hospitals. In particular, the difference in salary across both sectors is considerable.1 Although government hospitals are a more attractive option, nurses have to pass a competitive civil service examination to work there based on the current system. In India as a whole, nearly half of the nurse workforce is in the public sector. However, in some states, including Tamil Nadu, only a quarter of nurses work in the public sector (WHO 2021).
The Government of India recommends that the minimum wage for nurses at private hospitals should be 20,000 INR per month. Consequently, each state government sets the minimum wage for nurses working in private hospital. In the state of Tamil Nadu, it was set at a rate significantly lower than 20,000 INR. Further, our online interview survey on nurses in 2020 showed that not all nurses receive the minimum wages. Moreover, the number of nurses decreased in hospitals where the minimum wages were paid, so as not to increase the cost of hiring nurses. Further, nurses who work in the private sector during the COVID-19 pandemic were more willing to work abroad than those who work in government hospitals.
Recent Developments in the Public Sector
Owing to fiscal constraints, there is an increasing number of contract-based nursing positions in government health facilities for significantly lower wages and under much inferior conditions than nurses on permanent positions (Kurup 2012). Some nurses who were inactive were recruited to fill vacant nursing jobs in government hospitals during the COVID-19 pandemic. Nevertheless, there are still vacancies. Nurses are reluctant to take these vacant positions because the contract period during the COVID-19 pandemic was more likely to be shorter than usual, particularly 1 to 3 months (Johari 2021). This further contributes to the existing shortages of nurses, as potential nursing staff prefers to be unemployed or await recruitment into permanent positions instead of working with low wages and inferior working conditions in government health facilities.
Further, fiscal constraints have affected employment conditions among nurses with permanent contracts in the public sector. For example, the state pension schemes have changed from a statutory scheme to a contribution and operation one. Vacant positions are not always filled immediately. As the relative advantages of a government job in terms of salary and working conditions are eroded, nurses in government health facilities might seek overseas employment. There are some nurses with permanent contracts who joined state services. They took a leave, worked abroad, and did not return for a long time after their government job has been secured and the probation period was completed.
Implications for the Post–COVID-19 Era
With the COVID-19 pandemic, the pre-pandemic global shortage of nurses has exacerbated. Increased burnout and stress adversely affected nurse retention. Many developed countries have taken various actions to help migrant nurses to meet the sharp increase in demand for health care. These include accelerating new recruitment, facilitating the renewal of employment authorization, fast-track processing of foreign qualification recognition, and accepting people with temporary license (OECD 2020).
Accordingly, many Indian nurses have left the country during the COVID-19 pandemic. Our studies showed that if the working conditions of hospitals are poor, nurses in India are more likely to seek overseas employment. However, in recent years, better jobs in terms of salary and working conditions are eroded, and a larger-scale exodus of nurses from India might ensue. This is beleaguered further by the shortage of nurses. Unless a decent pay is ensured and working conditions are improved, India will remain one of the main suppliers of nurses worldwide. Indeed, Indian nurses are ready to serve different countries worldwide.
Author’s Note
This column is based on the following papers:
Oda, Hisaya, Yuko Tsujtia, and Sebastian Irudaya Rajan. 2018. “An Analysis of Factors Influencing the International Migration of Indian Nurses.” Journal of International Migration and Integration 19 (3): 607–24. https://doi.org/10.1007/s12134-018-0548-2
Tsujita, Yuko, and Hisaya Oda. 2023. “Nurse Education, Employment and International Migration: The Case of India.” In Nurse Migration in Asia, Emerging Patterns and Policy Responses, edited by Radha Adhikari and Evgeniya Plotinikova. Abington and New York: Routledge (forthcoming). https://www.routledge.com/Nurse-Migration-in-Asia-Emerging-Patterns-and-Policy-Responses/Adhikari-Plotnikova/p/book/9781032075136
Note
1: This is widely observed in different parts of India. For example, in Maharashtra, nurses in several private hospitals receive a monthly salary of 2,500–6,000 INR. Meanwhile, senior nurses in state hospitals earn 80,000 INR per month (Times of India 2016). In Delhi, smaller private hospitals pay 12,000–15,000 INR, and newly recruited nurses in state hospitals can earn 60,000–70,000 INR with various allowances (Times of India 2019).
References
Anand, Sudhir, and Victoria Fan. 2016. The Health Workforce in India. Geneva: World Health Organization. https://apps.who.int/iris/handle/10665/250369
Irudaya Rajan, Sebastian, and Sreelekha Nair. 2013. Assessment of Existing Services for Skilled Migrant Workers: India Project Site, ILO Promoting Decent Work Across Borders: A Pilot Project for Migrant Health Professional and Skilled Workers. Draft Report submitted to International Labour Organization.
Johari, Aarefa. 2021. “India is Hiring Nurses Monthly Contracts to Fight against COVID-19. The Jobs Have Few Takers.” Scroll in, May 9 2021, https://scroll.in/article/994367/low-pay-high-risk-no-security-why-india-has-failed-to-hire-more-nurses-to-fight-covid-19 (Accessed October 22, 2022.)
Kurup, Deepa. 2012. “Angels of Mercy Themselves Need a Lot of It.” The Hindu, March 20 2012, https://www.thehindu.com/news/cities/bangalore/angels-of-mercy-themselves-need-a-lot-of-it/article3015693.ece (Accessed October 22, 2022.)
OECD (Organisation for Economic Co-operation and Development). 2020. Contribution of Migrant Doctors and Nurses to Tackling COVID-19 Crisis in OECD Countries. OECD Policy Responses to Coronavirus (COVID-19). Paris: OECD Publishing. https://www.oecd.org/coronavirus/policy-responses/contribution-of-migrant-doctors-and-nurses-to-tackling-covid-19-crisis-in-oecd-countries-2f7bace2
———. 2022. Health Statistics 2022. https://www.oecd.org/els/health-systems/health-data.html
Times of India. 2016. “Now, Equal Pay for Private and State-Run Hospital Nurses, Recommended Committee Set up by the Indian Nursing Council.” September 23, 2022, https://timesofindia.indiatimes.com/city/mumbai/now-equal-pay-for-private-and-state-run-hospital-nurses-recommends-committee-set-up-by-the-indian-nursing-council/articleshow/54471610.cms (Accessed October 22, 2022.)
———. 2019. “Delhi: Nurses Make Less than Your Plumber.” December 5, 2019, https://timesofindia.indiatimes.com/city/delhi/nurses-make-less-than-your-plumber/articleshow/72374665.cms (Accessed October 22, 2022.)
WHO (World Health Organization). 2020a. Nurses and Midwifery. March 18, 2020, https://www.who.int/news-room/fact-sheets/detail/nursing-and-midwifery
———. 2020b. Status of World’s Nursing 2020: Investing in Education, Jobs and Leadership. Geneva: WHO. https://www.who.int/publications/i/item/9789240003279
———. 2021. Health Workforce in India: Why, Where and how to Invest? Geneva: WHO. https://apps.who.int/iris/handle/10665/350946
*Thumbnail image: triloks/ E+/ Female nurse examine patient lying on hospital bed (Getty Images).
**The views expressed in the columns are those of the author(s) and do not represent the views of IDE or the institutions with which the authors are affiliated.